If you are one of the tens of millions of people who experience clinical depression or bipolar disorder, you probably know what it’s like to feel shitty about yourself, irritable about interactions with others, afraid of what people might think about you, and hopeless about being able to do anything about it. You might also feel angry and frustrated – maybe even a sense of being trapped inside your feelings, with no way out.
Suddenly, what was pleasurable feels prickly, and people you may have felt connected to feel distant and irritating, like they “just don’t get you.” Maybe this leads to you wanting to retreat, to isolate, to push people away.
These are extremely hard feelings to bear alone, and yet that’s what depression encourages from you: to break healing connection because you feel, on some level, already disconnected and overwhelmed.
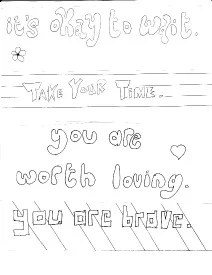
If you take pause in your feelings, either while they’re happening or soon thereafter, you may find you’ve been feeling this way for much of your life—perhaps not in any way you could name, exactly, and maybe you feel this way intermittently—but it’s as familiar to you as it is unfamiliar to people who do not have bipolar disorder or clinical depression. There’s no such thing as “normal,” but there are ways you can manage your depression and negotiate its “hooks” in you. Although the feeling is pervasive and often overwhelming, and it colors the way you see yourself and the world around you, it is possible to get to know it, and give yourself and these feelings the attention you both need.
Go into the feeling, and find where it resonates in your body. Spend some time with this exercise when you feel the irritability and sadness coming on:
1. Lie on your back in a quiet spot, and allow your breathing to settle however it wants to. Find the places your breath settles in your body; notice your chest rise, notice your shoulders, notice the muscles in your face and neck. Just notice, don’t try to change.
2. Allow your breath to explore your body, and notice what it finds. Breathe into different parts of your body: Your chest, your shoulders, your belly, your arms and fingertips, your hips, your back, and with each breath allow an exploration of tightness and resistance to happen.
3. When you find places that feel tight, achey, itchy, or uncomfortable, allow your breath to reach in and touch the tightness; on the out-breath, allow your body to let go. We’re not trying to “get rid” of the tightness or pain, just trying to make room to connect to it. You may spend a few breaths on the tighter parts of your body.
4. When you find these tight or resistant areas, in between your in-breath and out-breath, ask them: What do you need right now?
5. Then ask, How can I help you?
6. It may take some time, and quite a few breaths, to sit with the spots you discover and ask these questions. Just allow your breath to move, notice your pain and tightness, and ask for permission to know it.
7. When you are ready, slowly allow some movement back into your body and allow yourself to come back into the room.
When your awareness and attention have come back into the room, I encourage you to write down any sensation and any feelings you may have. Don’t worry about censoring yourself, just write.
This can be a very evocative exercise for people, and you may find a range of feelings. You may also find that nothing happens, which can also be evocative for some of us. If that’s the case, I encourage you to meditate on the “nothing,” because there is information there, too. Sometimes, “nothing” is a way to protect you from a deep sadness or trauma. Processing this experience in therapy can sometimes feel safer than doing it on your own, so I encourage you to bring your feelings about this exercise to your therapist, who can help you sit with things that might feel uncomfortable to do on your own.
For more information about depression or bipolar disorder, and to find community who shares these or similar experiences, take a look at The Neurodiversity Paradigm and The Icarus Project. This post is not meant to diagnose, treat, or prevent any disease. To begin therapy with a licensed professional with expertise in many types of mood disorders, give me a call at 510-594-4035 for a free phone consultation. I can point you toward resources that can be helpful to you in this process. It may take at least 24 hours for me to respond to your call, so if you or your loved one are suicidal or in crisis, take it seriously and call 911 or go to your nearest emergency room immediately. If you or your loved one are contemplating suicide, go to http://www.suicidepreventionlifeline.org/ or call 1-800-273-8255 to speak with someone 24 hours a day.
I provid e therapy in Berkeley, CA to individuals looking to delve into old patterns, explore overwhelming emotions, and find room for self-love and self-care amidst a harsh and unforgiving inner critic.
e therapy in Berkeley, CA to individuals looking to delve into old patterns, explore overwhelming emotions, and find room for self-love and self-care amidst a harsh and unforgiving inner critic.
To cite this page: Merson, M. (2014) Getting to Know the Harder Feelings of Depression and Bipolar Disorder. Retrieved month/day/year from http://mollymerson.com/2014/07/26/getting-to-know-the-harder-feelings/